EmblemHealth Replaces GHI Plans with New PPO Structure
EmblemHealth's partnership with UnitedHealthcare signals major network changes for Long Island employers. If you offer Emblem group plans, verify how this PPO transition affects your employees' access to care.

EmblemHealth just replaced its GHI plans with a new PPO structure, partnering with UnitedHealthcare for claims administration. While this change initially targets NYC municipal employees, it signals broader network consolidation that could impact Long Island small businesses offering EmblemHealth group coverage.
The transition took effect January 1, 2026, replacing the previous Emblem/GHI + Anthem/Blue Cross arrangement with the New York City Employees PPO Plan. For Nassau and Suffolk County employers, this matters because carrier consolidations rarely stay isolated to one market segment.
What Long Island Employers Need to Check
If your business offers EmblemHealth group plans, review your recent plan documents for any administrative changes. Carrier partnerships often mean shifts in:
- Provider network composition and access
- Claims processing procedures and timelines
- Prior authorization requirements
- Member service contact information
The financial impact depends on whether your employees' preferred doctors remain in-network under the new arrangement. Out-of-network surprises can trigger employee complaints and potentially affect your retention efforts.
Why Network Changes Hit Small Businesses Harder
Unlike large corporations with dedicated benefits staff, small businesses rely on employees to navigate their own healthcare decisions. When networks change without clear communication, you get the frustration calls—not the insurance company.
This is especially problematic for Long Island medical practices, dental offices, and professional service firms where employees often have established relationships with specific specialists. Comprehensive benefits guidance helps prevent these disruptions from becoming retention issues.
The Broader Consolidation Trend
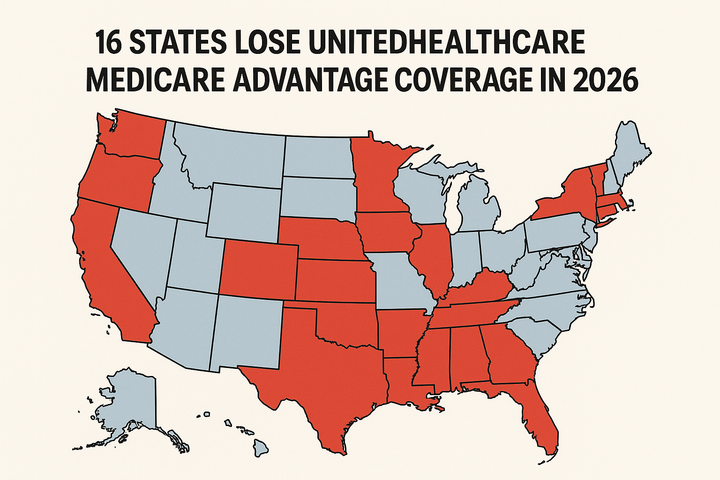
EmblemHealth's partnership with UnitedHealthcare reflects industry-wide consolidation. Smaller carriers are increasingly partnering with larger networks to compete on provider access and administrative efficiency. For employers, this means more frequent plan structure changes and the need for ongoing benefits oversight.
Without professional guidance, these transitions can create gaps in coverage understanding. Employees may assume their benefits remain identical when significant backend changes have occurred.
Action Items for Long Island Employers
Don't wait for employee complaints to discover network changes. Review your current EmblemHealth plan documents and verify:
- Whether your employees received updated provider directories
- If any administrative processes changed for claims or approvals
- Whether member service contact information remains current
- How these changes might affect your upcoming renewal discussions
For businesses approaching their renewal period, this transition highlights the importance of annual plan reviews. What worked last year may not provide the same value under new administrative structures.
Rather than reacting to changes after they impact your workforce, proactive benefits management keeps you ahead of carrier consolidations and network shifts. Benton Oakfield monitors these industry changes specifically for Long Island employers, ensuring your group plans adapt without disrupting your operations or employee satisfaction.
Compliance Note: Benefit plan rules and tax implications vary based on company size and location. This summary is for informational purposes only. Please contact your Benton Oakfield representative to review how these changes impact your specific plan documents.
Photo by Tima Miroshnichenko on Pexels