NewYork-Presbyterian Exits UnitedHealthcare Network March 31
NewYork-Presbyterian's March 31 deadline to exit UnitedHealthcare networks forces Long Island employers to prepare for April 1 out-of-network status that could increase employee healthcare costs 300-400% for major procedures at this major hospital system.
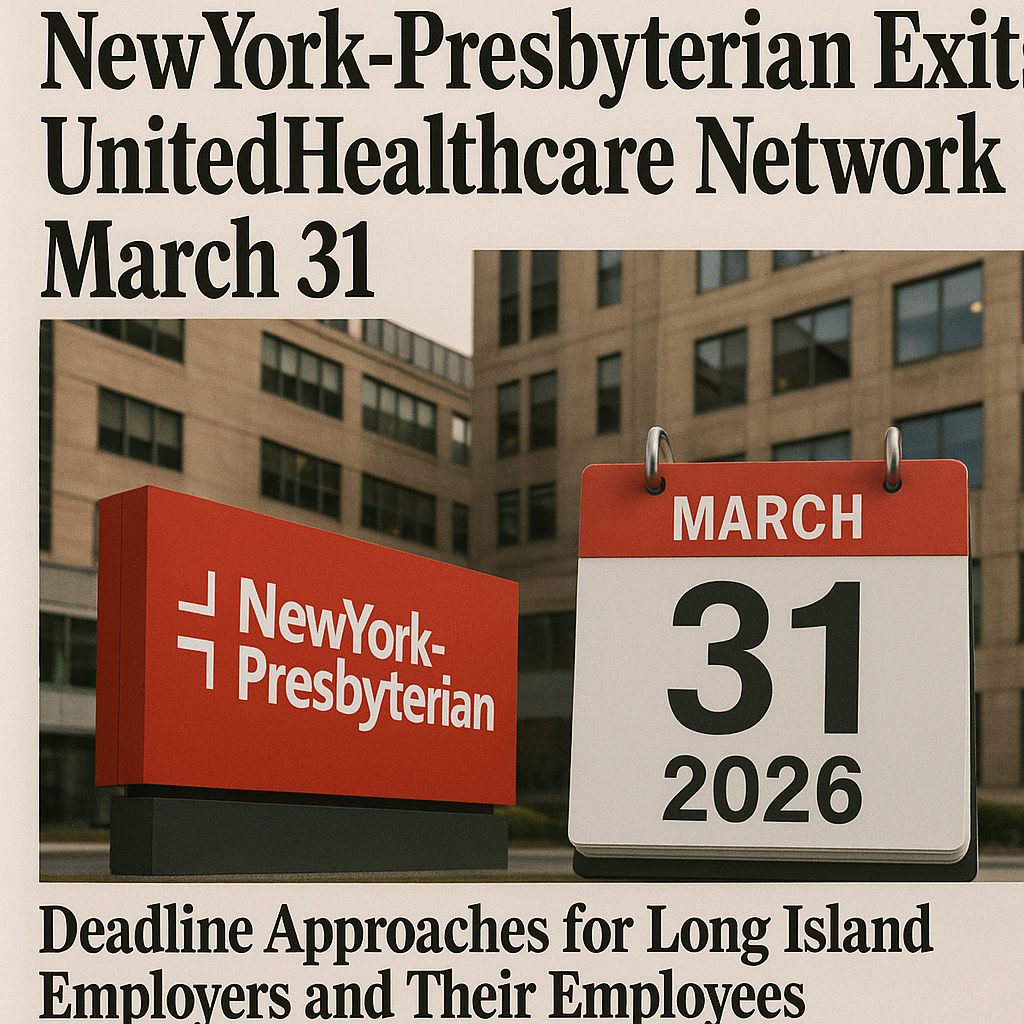
NewYork-Presbyterian's March 31 deadline to exit UnitedHealthcare networks creates immediate financial crisis for Long Island employers whose employees depend on this major hospital system for specialized care. The hospital system's final deadline for contract negotiations means that starting April 1, 2026—just 49 days away—employees with UnitedHealthcare coverage will face out-of-network charges that can be 300-400% higher than current in-network costs for major procedures, emergency care, and specialist services.
The network dispute affects all NewYork-Presbyterian facilities, including Columbia University Irving Medical Center, NewYork-Presbyterian Hospital-Columbia, NewYork-Presbyterian Hospital-Weill Cornell, and NewYork-Presbyterian Hospital-Allen, which serve as primary referral centers for complex cases throughout the NYC metropolitan area. For Nassau and Suffolk County employers with UnitedHealthcare plans, this creates immediate budget exposure: a single employee requiring cardiac surgery at NYP could generate $150,000-$200,000 in out-of-network costs compared to $50,000-$60,000 for equivalent in-network care.
The timing creates additional pressure during Q1 when Long Island businesses are completing ACA compliance deadlines and managing post-enrollment administrative tasks. NYP already went out-of-network for UnitedHealthcare individual plans on January 1, and the March 31 deadline affects commercial group plans, Medicare Advantage, and Medicaid coverage—forcing employers to make emergency decisions about coverage alternatives while managing other compliance priorities.
Immediate Financial Impact on Long Island Employers
The potential April 1 network exit creates three immediate cost pressures for Nassau and Suffolk County businesses: massive out-of-network claims that affect experience ratings, emergency plan changes that typically cost 20-30% more than standard renewals, and potential mid-year carrier switches that eliminate renewal timing leverage. A typical 40-employee medical practice could face $80,000-$120,000 in additional annual costs if just 2-3 employees require ongoing NYP specialist care at out-of-network rates.
Professional service firms face particular exposure because their employees often have established relationships with NYP specialists for complex conditions requiring ongoing care. When these providers go out-of-network, employees either continue treatment at dramatically higher costs or disrupt established care relationships to find in-network alternatives—both outcomes create employee satisfaction issues that can affect retention and productivity.
The claims impact compounds over time because NYP serves as a tertiary referral center for complex cases that generate high-cost claims. Employees with cancer, cardiac conditions, or other serious illnesses often require NYP's specialized services that aren't available through other in-network providers. Out-of-network treatment for these conditions can generate $100,000-$300,000 in additional annual claims per affected employee.
Emergency care presents another immediate concern. NYP operates several emergency departments throughout the region, and employees seeking emergency treatment at these facilities after April 1 will face significant out-of-network charges. Emergency room visits that currently cost $2,000-$3,000 in-network could result in $8,000-$12,000 out-of-network bills that create financial hardship for employees and potential liability issues for employers.
Employee Disruption and Care Continuity
The March 31 deadline forces employees with ongoing NYP care relationships to make difficult decisions about treatment continuity versus financial protection. Patients undergoing cancer treatment, managing chronic conditions, or scheduled for procedures at NYP facilities face potential care disruption that can affect clinical outcomes and create significant stress during already challenging health situations.
Long Island employers must prepare for increased employee inquiries about coverage alternatives, provider transitions, and financial assistance options. HR departments typically see 3-4 times normal benefits-related calls during network disruptions, requiring additional administrative support and clear communication protocols to manage employee concerns effectively.
The disruption particularly affects employees with family members receiving care at NYP facilities. When spouses or children have established relationships with NYP specialists, the network exit can affect entire families and influence employment decisions as workers seek coverage that maintains their family's healthcare relationships.
Medical and dental practices face additional challenges because their employees understand healthcare delivery and may have professional relationships with NYP physicians. These employees often have strong preferences for specific providers and may view network changes as significant reductions in benefits value, potentially affecting job satisfaction and retention.
Strategic Response Options
With 49 days until the potential network exit, Long Island employers have limited time to implement comprehensive solutions. Emergency carrier switches provide the most direct solution but typically result in higher premiums and reduced negotiating leverage. Alternative options include implementing higher out-of-network cost-sharing that shifts financial burden to employees or absorbing increased costs while hoping for quick resolution of the contract dispute.
Emergency plan design changes might include implementing specific exclusions for NYP facilities, increasing out-of-network deductibles, or adding prior authorization requirements for NYP services. These changes reduce employer cost exposure but create additional administrative complexity and potential employee satisfaction issues during an already stressful situation.
Some Nassau and Suffolk County employers are exploring direct contracting arrangements with NYP or alternative providers that maintain care continuity while controlling costs. These arrangements require significant administrative investment and may not be feasible given the compressed timeline, but they provide options for employers with employees requiring ongoing specialized care.
The key is developing contingency plans that address multiple scenarios: successful contract resolution before March 31, temporary network exit with quick resolution, or permanent separation requiring long-term alternative arrangements. Understanding medical plan network implications becomes critical when major providers exit networks and create immediate coverage gaps.
Communication and Compliance Requirements
Network changes require immediate employee communications explaining how the NYP situation affects their coverage and what options they have for continued care. These communications must be accurate, timely, and provide specific guidance about finding alternative providers, managing potential cost increases, and accessing financial assistance programs if needed.
The communication timeline is critical because employees need advance notice to schedule necessary procedures before March 31 or transition care to in-network providers. Delayed communication creates liability exposure if employees incur unexpected out-of-network charges because they weren't properly informed about network changes and their options.
Long Island employers also need to review their Summary Plan Descriptions and other compliance documents to determine whether network changes require plan amendments or employee notifications under ERISA requirements. Emergency network changes often trigger documentation requirements that must be completed within specific timeframes to maintain compliance.
Employee communications should include clear information about alternative hospital systems and specialist networks available through UnitedHealthcare, financial assistance programs for employees affected by the network change, and procedures for obtaining prior authorization or coverage exceptions for continued NYP care in emergency situations.
Alternative Provider Network Analysis
Before making emergency plan changes, employers should conduct immediate analysis of alternative hospital and specialist networks available through UnitedHealthcare in the NYC metropolitan area. Key alternatives include NYU Langone Health, Mount Sinai Health System, Northwell Health, and Hospital for Special Surgery, each offering different specialties and geographic coverage patterns.
The analysis must identify which NYP services can be adequately replaced through other in-network providers and which specialties may require out-of-network treatment regardless of the hospital chosen. Some highly specialized services offered at NYP may not be available through other UnitedHealthcare network providers, creating ongoing coverage challenges even after employees transition care.
Geographic considerations become important because alternative providers may be less convenient for Long Island employees who previously accessed NYP facilities. Travel time and transportation costs can affect employee utilization of alternative providers and may require additional support or incentives to ensure employees access necessary care.
The provider analysis should also evaluate appointment availability and new patient acceptance at alternative facilities. Network disruptions typically increase demand for remaining in-network providers, potentially creating scheduling delays that affect employees' ability to maintain continuous care during the transition period.
Precedent and Industry Trends
The NYP-UnitedHealthcare dispute reflects broader trends in provider-carrier contract negotiations where reimbursement rate disagreements are leading to more frequent network disruptions. Similar disputes affecting thousands of patients have become increasingly common as healthcare costs rise and carriers seek to control expenses through reduced provider payments.
Long Island employers should expect continued network instability as providers and carriers adjust to post-pandemic cost pressures and changing healthcare delivery models. The NYP situation demonstrates the importance of network stability analysis in carrier selection and the need for contingency planning that addresses potential provider exits.
The dispute also highlights the concentration risk that exists when employees develop relationships with specific hospital systems or specialists. Employers may need to consider plan designs that encourage broader provider relationships or include specific provisions for managing network disruptions that affect ongoing care relationships.
Professional service firms should monitor whether similar disputes affect other major providers in their employees' care networks. Network stability has become a critical factor in benefits planning that may require more attention than traditional metrics like premium costs or deductible levels.
Immediate Action Timeline
Week of February 10-16: Complete immediate impact assessment identifying employees currently receiving care at NYP facilities and evaluate emergency carrier switch options. Contact UnitedHealthcare representatives to understand their contingency plans and any updates on contract negotiations.
Week of February 17-23: Implement chosen strategy and begin employee communications about potential network changes. If switching carriers, complete applications and underwriting requirements immediately to ensure coverage continuity. If maintaining UnitedHealthcare, prepare detailed communications about alternative providers and cost implications.
Week of February 24-March 2: Finalize all plan changes and complete comprehensive employee communications. Ensure affected employees understand their options for continuing care and have information needed to transition to alternative providers if necessary.
Week of March 3-16: Monitor employee questions and provide additional support for care transitions. Coordinate with alternative providers to ensure smooth patient transfers and maintain care continuity for employees with ongoing treatment needs.
Week of March 17-31: Prepare for potential network exit by ensuring all administrative systems reflect new provider networks, employee communications are complete, and contingency plans are ready for implementation if contract negotiations fail.
Long-term Network Stability Strategy
The NYP situation highlights the importance of network stability analysis in benefits planning and carrier selection. Long Island employers should implement annual reviews of their carriers' provider relationships, contract renewal timelines, and potential disruption risks that could affect employee healthcare access.
Consider developing relationships with multiple carriers or implementing plan designs that reduce dependence on specific provider systems. This might include broader network options, direct primary care arrangements, or alternative funding strategies that provide more control over provider relationships and network stability.
The key is building flexibility into benefits strategies that can accommodate network changes without creating significant cost increases or employee disruption. Effective plan administration during network disputes requires proactive monitoring, clear communication protocols, and contingency planning that addresses multiple scenarios.
Nassau and Suffolk County employers should also consider the broader implications of network instability for their benefits strategy and whether current approaches provide adequate protection against provider-carrier disputes that are becoming increasingly common in the healthcare market.
Benton Oakfield's Network Crisis Response
Benton Oakfield's annual plan review identifies savings opportunities most employers miss when major network disruptions threaten employee healthcare access and employer costs. Our emergency response protocol provides Long Island clients with immediate analysis of network exits like the NYP situation, plus specific strategies to minimize cost impact and employee disruption while maintaining compliance with all federal requirements.
We're currently helping Nassau and Suffolk County employers navigate the NYP-UnitedHealthcare deadline with solutions tailored to their specific employee demographics and budget constraints. This includes emergency carrier evaluations, employee communication support, and contingency planning that addresses both immediate network changes and long-term stability strategies that protect against future provider-carrier disputes.
This content is for informational purposes only and does not constitute legal, tax, or benefits advice. Requirements vary based on employer size, location, and plan structure. Information is current as of 2026-02-10. Employers should consult qualified advisors for guidance on their specific circumstances.